Welcome to our Health & Wellbeing Advice Blog!
Here, you will find information about all things health and wellbeing.
Our weekly entries are full of engaging and useful information and resources.
From adults to children, rehabilitation to behaviour, movement to communication, we hope you will find this blog helpful.
Health & Wellbeing Advice
- What are visual schedules?
- Who can use them?
- How can they be used?
What is a visual schedule?
A visual schedule communicates the sequence of upcoming activities or events through the use of objects, photographs, icons, words, or a combination of tangible supports. A visual schedule can tell a child where they should be and what they should be doing. Visual schedules are designed to match the individual needs of a child and may vary in length and form and can be used in a variety of settings including school and home.
Visual Schedules and Reinforcers
Visual schedules support understanding by breaking down complex instructions. Children can refer to this for support during an activity and better understand the sequence of tasks. Visual schedules can also support attention and engagement as children understand expectations. Visual schedules and reward charts can be provided to support students to maintain attention to tasks.
Who can use a visual schedule?
Anyone! Any individual can use a visual schedule to help support the completion of daily activities in any environment!
How do you use a visual schedule?
-
- Identify the skill or routine you want to focus on. Breakdown the activity into steps. Choose a suitable visual format, this could be a “first- then” layout or a series of steps depending on the complexity of the task. Using photographs may be helpful for children to understand as they can easily associate the picture of an object to routine activity.
- Place the visual schedule in a location that is easy for the child to refer to throughout the activity or the day.
- Prior to starting the first activity or routine on the schedule, review all the upcoming planned activities with your child. Ensure the child is understanding what is required.
- Point out any unexpected changes in routine to ensure your child is aware of what is occurring/ going to occur.
- Point to the first routine and provide a verbal instruction, for example “The first task is to get your reader bag”. Providing this verbal instruction allows your child to process the information. If your child requires additional support, consider pointing in the direction which the activity or routine is to be completed or pointing or tapping on the task materials to assist your child’s understanding.
- Assist the completion of the activity or routine by providing assistance as necessary. This can be through simple verbal reminders or physical assistance.
- Provide positive reinforcement for following and completing routines independently (e.g. praise, such as “Great job coming to circle” or “Good sitting and painting”.)
Note: Include a reward/reinforcer as the final step to enhance motivation to complete the task.
Where to find a visual schedule:
You can download our Visual Schedule Template.
We have also included a variety of blank visual schedules below , so you can create your own schedule at home.
Alternatively, visit the Teachers Pay Teachers website for a range of Visual Schedules available for purchase.
Receiving extra support:
We hope this explanation on how to use Visual Schedules has been helpful. If you have any questions or concerns, please don’t hesitate to call our friendly reception staff!
Amelia Sharrad – Allied Health Assistant
7th June 2022
Play is an important and enjoyable way for children to stay active, improve wellbeing and develop important skills. Play is not only fun for children but is also an effective way to learn new skills required for thinking, language development, problem solving, creativity and emotional regulation.
What is imaginative play?
Imaginative play is when a child uses their imagination to role-play scenarios in a safe and fun environment. Imaginative play is open-ended and unstructured with no rules, goals or intended result. Examples of imaginative play include pretending to cook, saving the world, fighting bad guys, slaying dragons and more exciting adventures. There is no limit to imaginative play, it can involve props and costumes and be acted out anywhere.
Why is it important?
Imaginative play has a significant impact on children’s development and assists in improving their social and language skills, creativity and problem-solving abilities. Imaginative play also helps children understand and make sense of things that they have seen or experienced. It supports the development of creativity and intellectual development through use of imagination. It gives children opportunities to practice decision-making and social skills such as sharing and collaborating with others.
Along with this, imaginative play helps keep children active, promotes physical development and improves emotional wellbeing in a fun way. Activities such as dressing a baby doll assist with developing hand-eye coordination, and helps children learn to move and control their hands in different ways. Additionally, activities such as running around pretending to be a horse helps with gross motor development and coordination.
Finally, this form of play provides an opportunity for children to practice and develop their language and social skills by being with and talking to other children. Overall, imaginative play allows kids to relax, let go, and just be kids.
How to introduce imaginative play at home?
Below are some examples of imaginative play activities you can try with your children today.
The imaginative play ideas below can be used with your children at any time with little to no preparation or props required. Whilst it is encouraged that you support your child when they are engaging in imaginative play it is important that you do not begin imposing your own ideas and structure the play yourself.
- Become a chef and cook an imaginary meal
Bring out some pretend ingredients and get cooking.
- Have a tea party of a picnic
Invite along teddy and his friend and throw a wonderful tea party or picnic - Be a superhero or a bad guy
Be a villain and get up to some mischief or be a hero and save the day. - Get creative and make a box into anything
Find an old box and let your imagination run wild. Is it a bear’s cave or maybe a spaceship? - Put on a show
Make some puppets and put on a show. - Get gardening
Don’t have space for a real garden? No problem, grab some paper and pencils and make a fake garden complete with magic beans. - Run a café or a shop
Set up a market stall or grocery store counter and get selling. - Use your imagination
Anything can be used as an opportunity for imaginative play. Encourage your child to think creatively and follow along with their story line.
What to do if you have any concerns about your child’s play development?
If you have any concerns about your child’s play development, please don’t hesitate to call our friendly reception staff or jump on our website to join our waitlist today.
Amelia Sharrad – Allied Health Assistant

- Fluency vs disfluency
- What is a stutter?
- What therapy options are there for stuttering?
- Tips for talking with someone who stutters
FLUENCY VS DISFLUENCY
Fluency is how fast, accurate and expressive we say words so that we can be understood by others. Everyone has disfluent moments at times, especially when experiencing emotions or states such as anxiety, embarrassment, fear or fatigue. This normal disfluency is when we make 1-2 repetitions of a word (e.g. I want – want) or a phrase (e.g. I want to – I want to go home). These repetitions happen every now and then and do not interrupt the flow of conversation.
Children often show normal disfluency between the ages of 3-6 years old while they learn how to use language and speak in longer sentences. These disfluencies are expected to disappear as the child becomes more confident in their language skills. Children who speak more than one language may have an increased amount of normal disfluencies compared to those who speak one language during this time.
WHAT IS A STUTTER?
When a person’s disfluency begins to look like sound (s-s-s-stop), syllable (act-act-act-actually), word (in-in-in-in) or phrase repetitions with more than 2 repeats, stretching out/getting stuck on sounds e.g. ssssssssunny, or the mouth appears ‘stuck’ and there’s no breathing or sound coming out resulting in an unexpected pause e.g. I like ……..cooking. This is likely to be a fluency disorder called stuttering.
Other behaviours that can be observed with stuttering include using lots of filler words e.g., “um the um um dog is like like um running um away,” avoiding talking, excessive blinking, unexpected changes in pitch or loudness, and facial grimacing. The dysfluent moments occur one after the other and there is usually obvious tension in the face, neck and/or body as the person tries to get out what they’d like to say.
WHAT THERAPY OPTIONS ARE THERE FOR STUTTERING?
Two of the most common and evidence-based therapy programs for stuttering in children include the Lidcombe Program and the Westmead program. These programs are parent-led and includes 10-15 minutes of focus daily. Lidcombe program involves the parent commenting on the child’s speech whereas Westmead program involves the child speaking in the rhythm of the syllables in a word e.g. he-li-cop-ter.
Therapy programs for teenagers and adults include stutter modification (using strategies to modify stutters), smooth speech program (uses continuous airflow to change the speech pattern) and Camperdown Program (learning a novel speech pattern that is incompatible with stuttering).
TIPS FOR TALKING WITH SOMEONE WHO STUTTERS
- Speak to them in an unhurried way
- Show that you’re interested in what they have to say
- Allow them the time to speak with no interruptions
- Try not to tell them to slow down or relax
- Try not to finish their sentence for them
- Try not to make stuttering something to be ashamed of
- Ask them questions to clarify after they finished speaking if you struggled to understand them
- Encourage turn taking in conversations
- Acknowledge the stutters and let them know that it’s their brain working hard to keep time for all their words
Sarah Colangelo – Speech Pathologist
So you think you can dance?
There is often a misconception that the only way to exercise to reap any health benefits is going to the gym. However, not everyone enjoys this and it’s not the only way to move your body.
This year I have taken up salsa dancing and it has been so much fun, and definitely something I want to keep up!
Dancing is a great option for people of all ages, shapes and sizes. Even my 84-year-old Nanna is not opposed to a boogie from time to time! Dancing also has numerous benefits for both your physical and mental health.
Some of these benefits include;
- Improved muscular strength, endurance and cardiovascular fitness
- Promotes stronger bones and reduces risk of osteoporosis
- Improved coordination
- Increased flexibility
- Improved brain function
- Improved balance and spatial awareness
- Improved confidence and overall psychological well-being
- Improved condition of your lungs and heart
(Better Health Vic, 2022)
Dancing can also be great because you can do it in a group setting (i.e., dance studio, community hall, with friends etc.), with a partner or in the safety of your home. It is accessible for everyone! There are also a variety of styles that you can try from salsa, ballet, ballroom, disco, jazz or just your own moves that you have made up.
If this sounds like a form of exercise that you might enjoy but don’t know if it is suitable for you, book in to see one of our great physiotherapists or exercise physiologists and they can help you out!
Alison Harvey – Physiotherapist

Exercise is important for people at any age however is particularly important for children to help improve their wellbeing, gross and fine motor skills, balance and coordination, strength and fitness, communication and interaction skill and help to improve their overall quality of life.
What does exercise look like for children?
Exercises for children is not going to look the same as it does for an adult! As an adult we normally think of a structured exercise program which includes sets and reps however a child will often get bored completing this and won’t maintain motivation to continue. Therefore, exercise will look more like playing sport, playing games, playing on the playground, using imaginative play, etc. These will all still require the child to use gross motor movements to complete the required task of the activity and will allow the child to have some fun whilst doing so.
Why is exercise important?
Exercise has a significant impact on a child’s wellbeing. It can help with a child’s physical health such as improving their cardiovascular endurance, strength, balance and coordination. It can also encourage a healthy growth and development and a better posture.
Exercise has also been proven to not just help kids physically but also mentally with lowering their stress levels, improving their self-esteem, improving academic scores and increasing concentration levels. It additionally gives a child an environment to socialise and communicate with other people learning social cues and general communication skills. Lastly it increases a child’s energy expenditure which can encourage a better night sleep.
How to introduce exercise at home?
Below are some examples of exercise-based activities that you can try with your children.
Be mindful that not all children will enjoy all of these ideas, you will need to try a few and see what your child likes best.
- Play on a playground – Encourage them to use all equipment – climbing ladders, monkey bars, swinging, etc.
- Ball Sport Play – Ball sport such as basketball, soccer, netball, football, etc, all increase a child’s object control abilities as well as their balance and coordination. You can set up “goals” using mats, pans, rope, etc.
- Obstacle course – This can be very simple around the house. Include jumping over something, crawling under something, running, balancing on a line. You can add in exercises to this as well! (e.g. Crawl under the table, climb over the box, complete 10 star jumps and run 1 lap around the house to the finish line)
- Card Games – An easy game is go fish! If someone guesses wrong and they have to “go fish” as well as having to pick up a card, they also have a punishment. For example, 10 squats. This can be implemented into any card game.
- Walk – Some children just really enjoy being outdoors! If you feel like they need something to do whilst you are walking though you can provide them with a checklist of things to find or take a photo of. For example, take a photo of a duck, a bird, a snail, a pretty rock, some grass, the number 5 (could be on a letterbox) etc.
What to do if you have any concerns?
If you have any concerns about your child’s exercise levels, strength, coordination, balance, or general fitness development please don’t hesitate to call our friendly reception staff!
Stephanie Curnow – Exercise Physiologist

Let us introduce you to The Bounce Back ‘Women’s Health’ Physiotherapy Department.
Hello and welcome from the Women’s Health & Pelvic physiotherapists, Fiona, Mel and Naomi. We are 3 Physio’s who are passionate about helping women solve their pelvic health needs and regain their confidence.
It’s been a busy month here in the clinic for us! This month has included Continence Awareness Week and Pelvic Organ Prolapse Awareness Month! Mel and Fiona have also undergone an intensive professional development training month, getting them equipped with all the skills necessary to deliver you a thorough and detailed assessment. This now means, thanks to popular demand, that Bounce Back Health is now offering more available time to consult those seeking women health expertise (which we are super excited about!).
With June being a huge month for Women’s Health; lets start with some fun facts. Did you know…
- 1 in 4 Australians over the age of 15 years experience bladder or bowel control problems. That’s 5 million Australians and it’s expected to grow to 6.5 million by 2030 (Not if we can help it!)
- 1 in 3 women who have ever had a baby experience incontinence
- Pelvic floor muscle exercises have been shown to prevent and treat incontinence at any age
- 70% of people with incontinence do not seek help
- Incontinence can have a long-term physical and emotional impact; affecting self-esteem, motivation and independence.
- Bladder and bowel control problems are NOT a natural part or ageing or having a baby
(Facts delivered from the Continence Foundation of Australia)
So please, come and see us! We delight in offering you the highest quality care and we strive to make you feel like your self again because EVERYONE DESERVES TO FEEL BETTER.
The Women’s Health Department at Bounce Back Health offer services relating to:
- Pre-natal, pregnancy & post-partum care
- Pelvic pain
- Musculoskeletal concerns
- Painful intercourse
- Pain associated with endometriosis
- Pelvic organ prolapse / pelvic heaviness or dragging sensation
- Urge and stress urinary incontinence
- Pilates
- Pelvic surgical rehabilitation
And much more
If you’d like to find out more about our Women’s Health Physiotherapy Department, find us on Instagram @bounceback_womenshealth where we share useful information and tips about all things Women’s Health.
Bye for now,
Your lady Physio’s
Mel, Fiona & Naomi

If this blog post brings up some difficult emotions for you, there are supports available:
- PANDA (Support for Perinatal Anxiety & Depression)
- Gidget Foundation Australia (Free telehealth for new and expectant parents)
- Lifeline (24/7 Mental Health Support)
Today we’re talking about Birth Trauma. This can be a heavy topic, and something that has touched the lives of many women and their partners.
From the 17th to 24th of July was Birth Trauma Awareness week. This year’s focus was Birth Injuries – these can be physical, psychological or a combination of both.
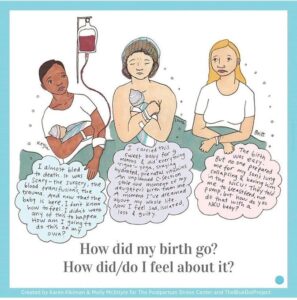
There’s ALOT to talk about when it comes to covering birth trauma and injuries – in this blog we’ll touch briefly on the type of injuries that can occur during birth, how physiotherapy can help, and what you can do to help prepare (physically and psychologically!) to reduce the risk of experiencing birth trauma.
It’s important to note that the term ‘Birth Trauma’ covers physical injuries as well as negative psychological effects from birth. Symptoms of psychological trauma can range from PTSD or postnatal anxiety/depression through to feelings of failure and feeling let down by the healthcare system. Having unexpected events happen such as your baby arriving prematurely, needing a NICU stay, or you requiring surgery can also seriously impact the way you experience birth and can leave long lasting emotional scars. Remember, YOU are the one that determines whether your birth was traumatic – no one else can determine that label for you. When you come to see us in the clinic carrying your birth trauma with you – we are here to listen. What you have been through mentally is just as important as the physical problem that has bought you to physiotherapy. We have 60 minute initial women’s health physiotherapy appointments for this reason – we want to hear YOUR story!
In terms of physical trauma – these are some of the physical injuries that can occur as a result of birth. If you have any of these injuries, a trip in to see us is going to be very beneficial to help you rehabilitate.
Perineal tears
These are classified by stages; Stage 1 (perineal skin), Stage 2 (skin and muscle), Stage 3 (skin, muscle and anal sphincter muscle), Stage 4 (skin, muscle, anal sphincter muscle and mucosa). Tears are repaired with stitches following delivery. A distressing result of having a tear extend to the anal sphincter can be faecal incontinence. However, some good news – the pelvic floor muscles and external anal sphincter are structures that can be rehabilitated.
Levator Ani avulsion
This is when part of the levator ani muscle (which makes up some of the pelvic floor muscle complex that supports your pelvic organs), is partially or fully torn away from its bony attachment on the pubic bone. Whilst we can’t re-attach the muscle with physiotherapy, we can help to strengthen the rest of the pelvic floor muscles and aim to prevent further issues from occurring, such as prolapse (see below!)
Pelvic Organ Prolapse
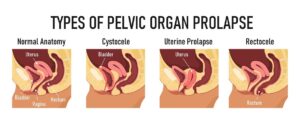 We won’t go into all the details about this one (it’s a blog post in itself!) – but sometimes after birth the pelvic organs (balder, uterus or bowel) can begin to press down and ‘bulge’ onto the vaginal wall, causing issues with pain, create feelings of heaviness or dragging and cause bladder and bowel symptoms. Prolapses aren’t always able to be diagnosed immediately at birth – but are something that we can look at, diagnose and help treat in the clinic.
We won’t go into all the details about this one (it’s a blog post in itself!) – but sometimes after birth the pelvic organs (balder, uterus or bowel) can begin to press down and ‘bulge’ onto the vaginal wall, causing issues with pain, create feelings of heaviness or dragging and cause bladder and bowel symptoms. Prolapses aren’t always able to be diagnosed immediately at birth – but are something that we can look at, diagnose and help treat in the clinic.
Other physical injuries and conditions that can occur during child birth include pudendal neuralgia (nerve damage), coccyx fractures, blood clots, infected stitches, bladder damage and excessive blood loss.
For readers who are pregnant or planning a pregnancy and are feeling anxious, scared or worried about Birth Trauma, we hear you! It can feel confronting to start looking at the types of injuries that can occur.

Time for some good news though – there are things you can do to prepare for birth that reduce your risk of physical injury!
This is bread and butter to us as women’s health physiotherapists and something we can help guide you through.
- Perineal massage to help relax and stretch the tissues of your perineum
- Pelvic floor muscle RELAXATION. Yes, strength is important… but so is being able to completely relaaax your pelvic floor muscles for baby to make his/her way through.
- Physical activity. It’s important for you to feel physically strong for labour and birth. Additionally, the more accustomed you and bubs are to having an increase in your heart rate during exercise, the better prepared you both are for exerting yourselves during labour.
- Stretching (hips, lower back, groin). Again, important for you to be nice and limber for the marathon of labour!
Mentally and psychologically, research and anecdotal evidence tells us that the following can also help:
- Ensure your birth preparation/education covers different types of deliveries (vaginal and caesarean, breech presentation, instrumental deliveries)
- Talk to your healthcare provider about your birth preferences
- Explore and practice the different types of positions you might like to try during labour – this is something we can help to give you ideas on!
- Practice mindfulness and repeat positive mantras/affirmations leading up to your labour
- Seek support if you are feeling overwhelmed and anxious about your delivery
If you need podcast, book, documentary or birth course recommendations to continue looking into physical and mental birth preparation please get in touch! We LOVE immersing ourselves in all things birth prep and birth education. As always, please DM us with any questions on Instagram @bounceback_womenshealth. You can also phone one of our clinics or book an appointment online with myself, Fiona or Naomi for an antenatal or postnatal assessment.
See you in the clinic!
Your lady physio,
Mel
Mel Clayfield – Women’s Health Physiotherapist
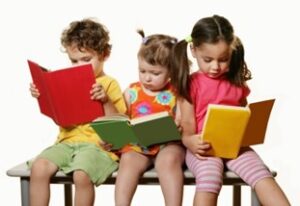
Books introduce your child to new worlds and can help your child learn language and build vocabulary. Book reading lays the foundation for reading and writing skills needed later in life. The earlier you begin to read and tell stories to your child, the sooner reading will become an important an enjoyable part of their life. Make reading a part of your everyday routine!
The importance of book reading:
Reading together with your child makes a huge impact on word exposure, which helps build their vocabulary and language skills. It is important to expose children to books from very early in their life in order to see a positive impact on their developing language skills.
Logan et al. (2019) correlated data from 60 commonly read children’s books to estimate the number of words that children are exposed to during book reading sessions for the first five years of life.
They found that on average, board books contain 140 word, and picture books contain 228 words.
Based on these numbers, here’s how many words children are exposed to by the time they turn five years old if they have been read to…
0 times (never read with): 4,662 words
1-2 times per week: 63,570 words
3-5 times per week: 169,520 words
1 book daily: 296,660 words
Multiple books per day: 1,483,300 words
Strategies for book reading with your child:
- You don’t have to start at the beginning of the book each time
- You can skip pages and not finish the book
- Don’t focus on reading stories word-for-word; take time to talk about the pictures and what is happening
- You can read the same book over and over again, even in one sitting! Repetition helps the child become more familiar with the book
- Use funny voices, sounds, exaggerated actions, and movements to go with the story to support the child’s attention and engagement
- Model sounds and words to accompany the story and pictures
- When the child is familiar with the story, pause at predictable parts for the child to fill in the blank
- Try to balance asking questions with reading the story, making comments or naming things in the pictures
- Let the child lead when reading books; follow their pace and let them look at each page in their own time. Talk about the things they are showing an interest in on the page
- Try not to rush through reading the story. Slow down your rate of speech to allow the child time to process what is being said, and to hear the individual words
- Use props (toys, household items, etc.) that complement the story. Show them and act the story out while you read it
- Reduce distractions; turn off background noise, put screens out of view, so you can focus on reading the book together
Alyce Carmichael – Speech Pathologist
The journey of a 32yo amateur superstar and running enthusiast to footballing premiership glory
Well, the title is probably misleading, I’m not a superstar, but I do play footy and I try to apply my physiotherapy and sports science knowledge to my life.
For anyone interested, so the 3 people still reading, here’s how I structure my week of exercise to include all facets of fitness, injury prevention and general health. For football I feel like I need strength, coordination, flexibility, power, muscular and cardiovascular endurance.

I’ve often thought that the key to keeping fit is finding something that motivates you and gives you happiness and accomplishment. I’m lucky because I weirdly love running and I love footy. A lot of people say I’m lucky to be fit but the truth is I actually work really hard for it. Here’s what I do:
My normal exercise week – A normal week would be 2 football trainings (around 5-10km each), a game of footy Saturday (roughly 14km), a Sunday recovery run between 5-10km, a Monday or Wednesday night-time run (3-6km), occasional bike rides and Wednesday morning swims of 500-1000m. The goal of my training here is endurance and coordination.
Strengthening – I’m lucky that through work I get to go to the gym with clients, so I sneak some strength training in. Every study in the last decade suggests that strength training is the key to injury prevention and performance so get onto that plz.
Conditioning – Through work I am lucky enough to do exercise sessions where I join in with clients. These are structed high intensity sessions where heart rates get up to 150ish for 20-30 minutes (think squat jumps, lunge jumps, battle ropes and core). These are good cardio blow outs, mixes things up and is good for muscular endurance and power.
Health – I’m no dietetics expert here but just a few simple things I do. Drink lots of water, diet cordial, eat lots of fruit during the day, lots of nutritious vegetarian meals, peanut butter toast every morning and lots of chocolate to treat myself. Lots of walking is key for mobility and flexibility (I walk my son Xander in the pram).
Pushing the limits – This is where I get a bit crazy. I like to do Parkruns on Saturday mornings in preseason or bye weeks (aim for sub 20minute 5kms). Did the Barossa half marathon a few weeks ago. Did 3x 20km trail runs earlier this year. Will do hills to Henley 30km run in July. I like running for the mental challenge and for endurance.
These are the things I do to keep fit. It’s not the perfect way, it’s just my way. And to be honest it makes me feel good pushing my body. In terms of footy, my team is undefeated 9-0 at the halfway point of the year. I’m keen to keep fit, taper off the running coming into finals and keep the good times rolling. Go TOS.
Brad Cameron – Physiotherapist
Let’s talk sensory!
Sensory regulation and emotional regulation are terms often used by our Occupational Therapists. But you may be wondering, what do they actually mean?
We hear you, these are often terms can be confusing and interchangeable, so lets break down what they actually mean first…
- Regulation allows children to respond to, change and manage emotions and arousal to match the activity or environment around them.
- Self-regulation, refers to ones ability to stay ‘self’ regulated, without the support of others, most children learn to do this naturally as they get older.
- Whilst Sensory Regulation, allows children to maintain an appropriate level of alertness in order to respond appropriately across environments to any type of sensory stimuli.
Now we know the terms, you may be thinking you have heard your therapist refer to using ‘sensory regulation strategies or a sensory diet’ to assist with a child’s regulation or self-regulation. Sensory regulation strategies, are essentially what the name suggests, strategies which use the bodies senses to help with regulation.

We thought it would be helpful to provide a small list of sensory regulation strategy ideas you may like to try at home with your child, to help either increase or decrease their arousal levels for optimal regulation throughout the day. Let’s have a look at some ideas for our 7 main senses:
- Tactile- Our sense of touch: Get your child engaging in sensory/messy play, water play and finger painting, provide massages and touch and feel books or try exploring play by walking barefoot on different surfaces e.g. grass, carpet, mud or sand.
- Auditory- Our sense of sound: Try having your child wear headphones in noisy environments, provide calming music/white noise at night, engage in meditation and singing.
- Olfactory- Our sense of smell: Use scented markers for drawing/colouring, diffuse essential oils, or use diffuser oil bracelets, ask your child to help with cooking and incorporate different smells.
- Visual- What we see: Use lava lamps or night lights with a warm orange or red colour, utilise sensory bottles, sand timers, dimmable lights and sunglasses in bright environments.
- Gustatory: Our sense of taste: Explore different textures, colours and tastes with your child- it may be useful to look into feeding therapy if you’re noticing excessive avoidance to foods. Use of oral chew toys, drinking through straws and chewing gum for children when safe to do so.
- Vestibular: Our sense of movement and balance: Swinging, spinning, rolling, somersaults, cartwheels and bouncing are all fun ways to incorporate these sense into the day!
- Proprioception: The sense our OT’s love! This is the sense of where the body is in space. Activities include that of pushing, pulling and carrying heavier objects, e.g completing wall push-ups, climbing on play equipment or playgrounds, eating crunchy foods, animal walks, obstacle courses and rolling up in blankets.
It’s Important to note, there is no ‘one size fits all’ when it comes to sensory regulation strategies. Some sensory regulation strategies will increase arousal, whilst others will lower it. It’s important to find ‘just the right’ mix for each child and provide sensory strategies at planned intervals throughout the day. This ensures there is an optimal level of regulation maintained throughout the day and not just provided when the child is already experiencing feelings of dysregulation.
This is called a ‘sensory diet or regulation plan’, meaning sensory strategies will be unique to each individual child. If you’d like to know more about sensory regulation and developing a sensory diet for your child, speak with your Occupational Therapists to explore what works best for you and your child!
Brianna Fuller – Occupational Therapist
When you’ve got a fussy eater it can make mealtime’s stressful, feel like a ‘battle’ and it can be easy to feel frustrated and powerless. Feeding is one of the most complex skills we can do! Did you know that feeding involves all our organs, all our muscles, all our senses? Eating is a reflex from birth until 6 months of age. After that eating is a learned behaviour. Sometimes children need additional support learning how to eat which is where a feeding therapy can be beneficial.
What is feeding therapy?
Feeding therapists are trained speech pathologists and occupational therapists who are specialised to work with those who have or are at risk of having feeding difficulties. Feeding therapy aims to help children broaden the range and types of food they eat, support with making mealtimes a positive experience, develop oro-motor skills (e.g. chewing, swallowing), help support sensory needs at mealtimes and develop a child’s confidence in exploring new foods.
Feeding therapy can help support children who:
- Have a restricted range of variety of foods
- Get distressed at the sight of unfamiliar foods
- Have extreme difficulty or refuses eating entire food groups or textures
- Eats separate meals to the family
- Are consistently described as being a ‘picky eater’

10 Strategies to support fussy eating at home
- Posture is important. Have your child‘s feet flat on the ground/stool when eating.
- Have family meals together. This is a chance to model good eating behaviours and for your child to see you eating new foods. Everyone sits down together and is offered the same food.
- Always provide at least 1 preferred meal at each mealtime.
- When serving new foods encourage your child to interact with it (e.g. touching it with cutlery or their fingers, smelling it or playing with it) without any pressure to eat it.
- Have a ‘learning plate’ where your child can put new foods if they are not yet comfortable having it on their own plate.
- Play with food! Pretend your carrot stick is a car and drive it round the table, use broccoli as a ‘paint brush’ and apple sauce as your ‘paint’ or use string cheese to make faces. Get creative and have fun!
- Get your child involved in cooking. Let them crack an egg or squeeze the orange juice. It’s a great way to interact with new foods.
- Make small changes to your child’s food to help them learn about the different properties of foods and to support them being more comfortable with different foods. Change the colour of the food by adding food dye, use cookie cutters to change the shape, change dips to try a new flavour, change the texture by comparing cooked carrots to raw carrots.
- Get everyone involved in the clean-up routine. It’s a great way for your child to be involved in interacting with new foods by picking it up to throw away or put in a container.
- Don’t give up! Keep trying a child may need to be exposed to a new food at least 10 times before they may try it or eat it.
What to do if you have any concerns about your child’s eating?
If you have any concerns about your child’s feeding development please don’t hesitate to call our friendly reception staff or jump on our website to join our waitlist today.

Caitlin Pywell – Senior Speech Pathologist
Episiotomies are a surgical incision made to the perineum (tissue between vaginal opening and anus) during childbirth. Two primary reasons why an episiotomy is completed is to assist widening the vaginal opening or if baby is experiencing fetal distress. Doing so ensures the safe delivery of little bubs and reduce the likelihood of unplanned perineal tears.
Prior to an incision, local anaesthetic is used to numb the area and a small, diagonal cut that is directed down and out is made. Generally, post-delivery, dissolvable stitches are used to close the incision site.
Perineal tears occur during childbirth where the vaginal opening isn’t big enough for the baby. These tears are not unplanned and are uncontrolled which can result in versions regress of tears. These tears are classified by stages;
Stage 1: perineal skin
Stage 2: skin and muscle
Stage 3: skin, muscle and anal sphincter muscle
Stage 4: skin, muscle, anal sphincter muscle and mucosa
Tears are repaired with stitches following delivery. A distressing result of having a tear extend to the anal sphincter can be faecal incontinence. However, some good news – the pelvic floor muscles and external anal sphincter are structures that can be rehabilitated.
Additionally, some things a women’s health therapists can do to try to help minimise the risk of perineal tears are;
- Perineal massage: combination of massaging and stretching the perineal muscles
- Warm compression during perineal massage and during crowning can help relax the area to reduce tearing
We hope this advice helps you soon to be mamas! And remember we’re always here to help!
For any questions, contact us on instagram @bounceback_womenshealth or book an appointment with Fiona, Mel or Naomi today!
Fiona Pham – Women’s Health & Pelvic Floor Physiotherapist
The shoulder is a complicated part of the body and a lot of individuals experience difficulties related to the function of their shoulder. For some it’s painful and difficult to move while others simply find it challenging to perform certain actions or movements in their shoulder which they used to be able to do without issues.
Today we are going to cover some basic information about how the shoulder moves and its relationship with our torso, how posture effects the shoulder movement, and some easy movements to help make movement with our shoulder easier and potentially reduce pain and discomfort.
There is a lot going on around the shoulder but we will keep it simple in this discussion.
The basics that you need to know are that the movement of the arm, from the shoulder come from two main places.
First is the shoulder joint itself which is where the arm bone (humerus) attaches to the shoulder blade. This joint produces most of the movement of the arm down below 90 degrees like when the arm isn’t over head.
Second is the shoulder complex as a whole which requires the shoulder blade to move and adjust. This then allows additional movement in combination with the shoulder joint.
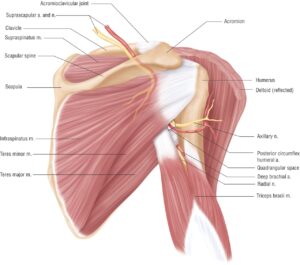
Part of why the shoulder blade must move is because if it didn’t, the bones like our collar bone and tip of the shoulder, would get in the way of the arm bone and jamming the bones against each other isn’t very comfortable.
So where does our posture come in?
Because our shoulder blade is attached to our torso and surrounded by all the muscles that move the shoulder it needs to slide and move around against the chest wall on the back.
Here is a simple test, (remember not to try if it’s painful).
Sitting up tall reach your hands up above your head. Now compare what happens if you slouch right forward, curving your back over and try reaching up again and see how far you can reach.
Not nearly as far right? And it’s not very comfortable either.
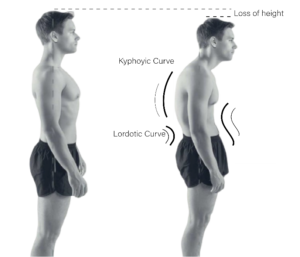
By slouching or stooping, like in the picture here, the shoulder blade can’t move like it’s designed to. This means it can’t move the shoulder like it should and it gets in the way of the arm bone so it makes sense that it’s not very comfortable.
So if you find your having difficulty or pain, try adjusting your posture first and see if it helps.
If you are having difficulty with your shoulder, book in with one of our physio’s. We can help you perfect these movements, improve your shoulder range, function and reduce your pain.
Mathieson Russell – Physiotherapist
Home modifications is the process of changing areas of the home in both structural and non-structural ways in order to support engagement in daily activities. Structural home modifications are changes that involve the load bearing elements of the home, including walls, floors and roofs. Non-structural modifications are changes that are able to be completed by single trade work and does not impact the load bearing elements of the home, including installing different taps in the bathroom, adding sensor lighting and changing the kitchen counters for higher contrast and extra grip.
Home modifications are important for allowing people to maintain independence in daily activities. When looking at activities completed throughout the day the environment is a major factor in achieving success in tasks. If the environment is too challenging for a person to safely and effectively participate in a daily activity then the environment can be changed. Without changes in the environment to assist with daily activities people struggle to maintain independence and require outside support from support workers or family.
The process of investigating, assessing and implementing home modifications is relatively simple. To begin talk to an OT about conducting a home assessment for the purpose of modifications. The OT will inspect the areas of the home that a person has identified as challenging areas and discuss options for changes in the environment. The OT takes measurements and completes diagrams to show the current home and proposed modifications. Once modifications are agreed upon a builder attends the home to confirm measurements and provide any additional suggestions for modifying the home. Then the OT completes a report conveying the need for home modifications and the cost of the modifications, which is provided to the person’s funding body for example, NDIS or MyAgedCare. When the funding body approves of the home modifications the builders are then responsible for organising and completing the works on the home. After the installation of the home modifications the OT will complete an assessment with the person to determine if the modifications to the home have assisted in the participation of daily activities.
Examples of different home modifications available and their benefits:
- A ramp installed at the front door with bilateral rails can assist people with mobility difficulties to enter and exit their home.
- Sensor light strips added from the bedroom to the bathroom can assist people with vision impairment make their way from the bedroom to the bathroom at night in order to use the toilet.
- Complex bathroom modifications such as changing the closed shower to an open circular shower with a curtain rod, adding rails by the toilet and in the shower, replacing the towel rail with a weight bearing rails, adding a handheld shower head to the shower and adding a shower bench can assist with people who have complex physical, developmental, sensory or cognitive disabilities to maintain independence in their personal care of showering, dryings, dressing and grooming.

If you are concerned about your or a family members ability to complete daily activities and believe that the home environment may be a contributing factor, visit our website and join the waitlist for home modifications under Occupational Therapy services.
Emma Holloway – Occupational Therapist
At Bounce Back Health, we are passionate about Pilates!
Pilates is a unique way of strengthening with a focus on deep stabilisation, flexibility and posture. It has been shown to have dramatic affects on our wellness. We love the way it can have an integral part on rehabilitating an injury, surgery or joint replacement, just to name a few! It’s a fantastic way to prepare for birth and recover in your post-partum period too.

Pilates is a great option for both men and women. Its unique structure allows us to strengthen and move with reduced impact on our joints. Don’t be fooled though, Pilates is no walk in the park! Quite often our clients, and we ourselves, are surprised at how challenging Pilates can be.
Pilates repertoire can be completed through both mat work of on a reformer. One is no more challenging than the other, they are simply undertaken differently. Both options have ability to be made easier or harder. Mat work is often assisted with small equipment in the form of a chi ball, Pilates ring or theraband to help you get that burn!

Similarly, reformer work can be challenged with small equipment, however the resistance is based on a spring and carriage system. Depending on the exercise, high spring load can make an exercise super easy or super hard! This is one of the many ways that Pilates surprises us and challenges us to new extents.
At Bounce Back Health we offer:
Group mat work classes including Mum’s & Bub’s mat work
-
- Tuesday 6pm
- Wednesday 6pm
- Thursday 6:30am
- Friday 10am
Private bookings at any time that suits you!
-
- One on one mat work sessions
- One on one reformer sessions
Our Pilates “gurus” at Bounce Back Health include our physiotherapists Alison, Cassie, Mel and myself, Naomi. Our reformer and classes operate out of our Gawler East clinic however one on one mat work sessions can be booked across all of our clinics.
I’d love to answer any of your questions concerning Pilates.
Feel free to ask on our Instagram accounts or via e-mail
E | nmanton@bouncebackhealth.com.au
IG | @bouncebackhealth or @bounceback_womenshealth
Happy Wednesday!

Naomi Manton – Women’s Health & Pelvic Physiotherapist
What is it?
Dry needling is a treatment where fine, sterile, single use needles are inserted into the muscle (piercing the skin) in order to stimulate a twitch response which releases or relaxes the trigger point (knot).
Dry needling is different to acupuncture but does share some similarities. Dry needling focuses on releasing myofascial trigger points in the muscle to reduce pain and help restore function. Acupuncture however is often used to treat medical conditions by restoring energy flow at specific points in the body.
What are the benefits of dry needling?
The use of dry needling as part of your treatment can assist in releasing trigger points/knots, decrease pain, and often help restore movement.

What to expect?
The treatment itself only lasts a few minutes. The sterile and single use needle is inserted into the skin and a ‘fishing’ or ‘pecking’ motion is used to stimulate the twitch response. The insertion of the needle doesn’t generally hurt. You will feel an ache with the twitch of the muscle and for most people the ache will continue for a few hours after treatment. If you have ever experienced a ‘corkie’ this is similar to the post needle effect. This ache will settle and movement will help with this!
Side effects
As with many treatment techniques there can be side effects. With dry needling your physiotherapist will go through these with you and may include minor bleeding and bruising, drowsiness, achy muscles.
Who can have it?
Almost everyone! However there are some who this treatment may not be suitable for. This includes those who have a higher risk of infection (eg post surgery), blood clotting disorders, or those that have a phobia of needles.
Pricing
We do not charge any additional fee’s for dry needling. If you have physiotherapy extra’s on your private health fund, this is a deductable service!
Sounds good, what next?
Here at Bounce Back Health both Fiona and myself (Cassie) are trained in dry needling. So if you think that dry needling would be a beneficial treatment addition or have further questions, contact our clinic to book a session!
Cassie Smiler – Physiotherapist
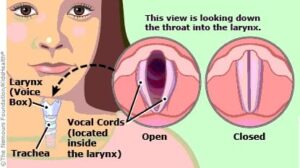
What makes up your voice?
The voice itself has a few important systems in play that help produce sound, but lets begin with the larynx, also known as the voice box. The larynx helps us with breathing, swallowing and of course producing sound (talking, singing, laughing, screaming). In order to actually get the voice producing sound we use 3 systems to get it all fired up and working!
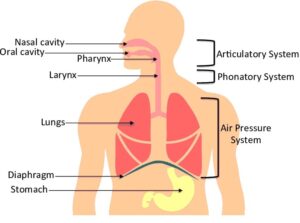
The Respiratory System is what we refer to when we talk about our breath support. It is made up of our windpipe, lungs, diaphragm, ribcage, and our surrounding muscles like the chest muscles and stomach muscles.
The Phonatory System is where the sound is actually produced through the larynx, also known as the ‘voice box’ with the use of vocal cords, also known as vocal folds.
The Resonatory System is known as the vocal tract that helps create the shape of the resonance through the nose, throat and mouth passages.
Vocal Cord Disorders
Vocal cord disorders are any anatomical or functional issue that affects the vocal cords. The vocal cords (also called vocal folds) are two bands of smooth muscle tissue found in the larynx (voice box). The vocal cords vibrate and air passes through the cords from the lungs to produce the sound of your voice.
Some of the more common vocal cord disorders include the following:
- Laryngitis
- Vocal Nodules
- Vocal Polyps
- Vocal Cord Paralysis
What causes vocal cord disorders?
The most common cause of vocal fold disorders is vocal abuse or misuse. The type of vocal cord disorder may have different causes. This includes excessive use of the voice when singing, talking, coughing or yelling. Smoking, some medications and inhaling irritants are also considered vocal abuse.
Who is at risk of vocal injury?
Voice disorders affect all ages, however, evidence suggests there is a higher prevalence in paediatric an elderly (over 65 years old) populations. It is estimated that 23.4% of children have vocal issues and most commonly boys ages 8 to 14. The risk is also significantly higher for adults with age-related vocal changes.
Finally, people in vocations with high vocal demands have increased likelihood of developing dysphonia. Including singers, legal professionals, entertainers, teachers, coaches and so on. Issues with the voice an impact an individual’s ability to work and function daily.
What are the symptoms of vocal cord disorders?
Symptoms vary, based on the type of vocal cord disorder. They include changes in your normal voice, such as a raspy or hoarse voice, or a hoarse, low and breathy voice. Vocal cord paralysis may also cause trouble swallowing and coughing.
To know how you are treating your voice, ask yourself the following questions:
- Do I use my voice more than I have to?
- Could I effectively use other methods to make my message understood?
- Do I use my voice as efficiently as I can?
- Can I speak at a quieter level during certain classroom activities?
- Is the layout of the classroom conducive to efficient voice use?
- Do I always talk above background noise?
- What is the source of the background noise and how can I reduce its impact on my voice use?
When you have determined the answers to these questions, consider what behaviour modification techniques you could employ to enhance the effectiveness and efficiency of your voice.
How to prevent/minimise voice strain
Often called ‘Vocal Hygiene or Health’, caring for your voice means learning to pay attention to the signals that your voice gives you so that you take the necessary steps to avoid getting injured in the first place. It also requires that you think ahead, learning to change certain behaviours which might lead to an injured voice e.g. improving how the larynx (voice box) works through voice therapy.
- Turn down, shut out, or move away from noise in the environment while talking.
- Use gesture and other non-vocal signals to give instructions such as clapping your hands to gain attention.
- Talk to groups or classes when the individuals are quiet.
- Stand in a place in the room that will make it easiest for the listenders to hear you without straining your voice.
- Avoid yelling or loud talking.
- Produce your speech sounds clearly and precisely and slow your speech so that listeners can understand you, minimising the need for you to talk very loudly or having to repeat yourself.
- Move close to listeners when talking to them.
- Sing only in a range and style that is comfortable for where you where possible.
- Plan the day so that you build in voice rest periods, where you do not need to talk.
- When outdoors or in large open areas, such as gymnasiums, use a megaphone or PA system to project your voice.
- Where supported by medical advice, use a voice amplifier.
Strategies to reduce the symptoms of voice strain
You can work on reducing the symptoms of voice strain by using strategies such as:
- Drinking water frequently throughout the day.
- Being conscious of your posture and breathing when speaking (back straight, head up and chin level with the ground).
- Sipping water, swallowing or yawning whenever you feel the urge to cough or clear the throat.
- Sucking on a sweet, but avoiding medicated lozenges, which may irritate your throat further.
- Consciously suppressing the urge to cough or clear the throat.
If you or someone you know is experiencing issues with their voice, contact our clinic today or chat to your local GP to find out more.
Amelia Sharrad – Allied Health Assistant
“Sex is painful but I just get on with it”
“I leak when I cough.. that’s just part of being a woman”
“It feels like my insides are falling out”
“My body just isn’t the same since I had kids”
These are all very common things we hear within in conversations with friends, family, our clients and also within wider society. Like we always say in the Bounce Back Women’s Health department.. just because something is COMMON, doesn’t make it NORMAL! There are so many things we can do to help with pelvic symptoms of pain, incontinence and prolapse.
 If you’re still not quite sure if we can help you – have a look at this great screening tool below. It aims to tease out whether you may benefit from assessment with a women’s health physio.
If you’re still not quite sure if we can help you – have a look at this great screening tool below. It aims to tease out whether you may benefit from assessment with a women’s health physio.
If you answer ‘yes’ to three or more of these statements, it’s likely you have a level of dysfunction that we can assess and assist you with!
- I sometimes have pelvic pain (in genitals, perineum, pubic or bladder area, or pain with urination) that exceeds a ‘3’ on a 1-10 pain scale, with 10 being the worst pain imaginable
- I can remember falling onto my tailbone, lower back, or buttocks (even in childhood)
- I sometimes experience one or more of the following urinary symptoms
- Accidental loss of urine
- Feeling unable to completely empty my bladder
- Having to void within a few minutes of a previous void
- Pain or burning with urination
- Difficulty starting or frequent stopping/starting of urine stream
- I often or occasionally have to get up to urinate two or more times at night
- I sometimes have a feeling of increased pelvic pressure or the sensation of my pelvic organs slipping down or falling out
- I have a history of pain in my low back, hip, groin, or tailbone or have had sciatica
- I sometimes experience one or more of the following bowel symptoms
- Loss of bowel control
- Feeling unable to completely empty my bowels
- Straining or pain with a bowel movement
- Difficulty initiating a bowel movement
- I sometimes experience pain or discomfort with sexual activity or intercourse
- Sexual activity increases one or more of my other symptoms
- Prolonged sitting increases my symptoms
Our instagram inbox is always open if you have any questions about our services @bounceback_womenshealth. Book online or phone our friendly admin staff on 08 8520 6244 if you’d like to book an appointment!
See you soon,
Mel Clayfield – Physiotherapist
Reference: Cozean Pelvic Dysfunction Screening Protocol (2018)
As an Exercise Physiologist, my clients always ask me “how long will it take to see results?”. And it’s a good question!
Whether they want to build muscle or to run 5K in a set time, everyone is looking for RESULTS. If you’re curious about how your body responds to exercise (and how long it takes to see changes), then read on…
Remember, to get results, you need to do ‘regular physical activity’. This means doing at least 30 minutes of physical activity on most days of the week. If you can’t, then try to be as physically active as you can in your current state of health. Any activity is good activity, and something is always better than nothing.

HOW LONG DOES IT TAKE TO SEE RESULTS?
HEART RATE: CHANGES WITHIN A COUPLE OF WEEKS.
The heart is a muscle, and as you get fitter, it will become stronger. Over time, this means your heart will pump more blood per beat than before. This can, in turn, decrease your resting heart rate.
Resting heart rate can decrease by up to 1 beat/min in inactive individuals with each week of aerobic training (i.e. exercise that makes you huff and puff), at least for a few weeks. Other studies have shown smaller reductions with fewer than 5 beats following up to 20 weeks of aerobic training.
Your maximum heart rate typically stays unchanged with regular training and is more likely to decrease over time as part of the normal ageing process.
People who are fitter also tend to have a heart rate that recovers faster after exercise.
BLOOD PRESSURE: CHANGES IN A FEW WEEKS.
Exercise causes moderate reductions in blood pressure (BP) in those who have borderline or moderate levels of high blood pressure.
One study showed that simply increasing your step count can lead to a reduction in systolic blood pressure of ~4 mmHg. This may seem small, but a 5 mmHg drop reduces the chance of death by stroke by 14%!
Individuals with blood pressure in a ‘normal’ range don’t normally notice a change in their BP at rest or with exercise.
AEROBIC FITNESS (AKA VO2MAX): CHANGES IN A MONTH OR TWO.
VO2max, which is the highest rate of oxygen consumption possible during maximal or exhaustive exercise, is a great indicator of someone’s physical fitness. With endurance training our body can deliver more oxygen to the working muscles allowing it to do more for longer and with reduced effort.
Improvements range from 5-30% with a regular, sustained program. Untrained individuals can see improvements of 15-20% in their VO2max following a 20-week aerobic training program. This allows them to perform an activity (e.g. running) at a higher intensity for longer.
MUSCLE FITNESS: EXPECT TO SEE SMALL CHANGES IN THE FIRST FEW WEEKS.
Within three to six months, an individual can see a 25 to 100% improvement in their muscular fitness – providing a regular resistance program is followed.
Most of the early gains in strength are the result of the neuromuscular connections learning how to produce movement. Sometimes accounting for up to 50% of strength improvements in the early stages of a strength-based program.
Changes in muscle size from resistance training are highly variable – from no change at all up to roughly 60% increases with a long-term resistance program.
WEIGHT LOSS: RESULTS WITHIN WEEKS.
Exercise can be used as an effective tool for weight loss and preventing weight gain. People wanting to lose weight should aim to be physically active for 60+ minutes per day to notice any significant changes. It also needs to be at a moderate intensity.
One study with 52 obese males reported a body weight decrease of 7.5kg over 3 months using only exercise. Participants did ~60 minutes of exercise per day with a goal of 700 calories (~2940kJ) expended.
Another study with 52 overweight males and females reported a weight loss of 7% over 16.8 weeks with exercise alone. The amount of activity completed was 7.4 (+/- 0.5) hours per week.
MENTAL HEALTH: CHANGES IN AS LITTLE AS 10 MINUTES!
While there are numerous physical benefits from regular physical activity, it also benefits our psychological health too. Even brief walks, at a low intensity, can improve our mood and energy levels. You can start to notice positive effects after as little as 10 minutes of aerobic training.
If you’re interested to know more about the benefits of regular activity and getting results, then get in touch with one of the Exercise Physiologists at Bounce Back Health.
Harry Beresford – Exercise Physiologist
Blog post adapted from https://exerciseright.com.au/how-long-exercise-results/ which was written by the same author.
What is interoception?
Did you know our body constantly sends signals to let us know how we’re feeling. Do you feel your stomach growl? Your palms sweat? Your heart pounds? Tingles in your body when you’re nervous? These are all part of interoception awareness. This secret sense is responsible for what’s going on inside our body. It helps us be aware when we are hungry, when we need to go to the toilet, temperature changes in our body, stomach aches, headaches and many more. Interoception is one of the major senses, just like our vestibular, proprioception, smell, sight, sound, taste and touch.
Interoception and self-regulation
Interoception can also help us identify different emotions in our body. This is separated into two categories, affective emotions and homeostatic emotions.
Affective emotions: Emotions that regulates our moods and reactions to the environment. These include simple emotions such as happy, angry, sad, worried to more complex emotions including jealousy, irritation, embarrassed, annoyed and more (Mahler, 2019).
Homeostatic emotions: Emotions that tells us when we are hungry, thirsty, feeling sick, urinating and sleeping. Other homeostatic emotions that we may feel may include but not limited to nausea, constipation, sensory overload, sexual arousal, pain, exhaustion and more (figure 1).
These emotions have a significant impact on our ability to self-regulate. In order to become aware of our emotions and self-regulate we first need to be able to notice our body. For example, “what body signals am I noticing right now?”, “Is my head throbbing or is my stomach churning?”. Next, we need to connect with our emotions. This is a crucial step before we begin to self-regulate. During this step, we begin relating our body signals to our emotions such as “what do my body signals mean” and “what emotion am I experiencing”. The final step is to regulate and act. This is when we identify what we need to keep the comfort or restore the comfort within our body.
According to Kelly Mahler (2019), noticing the way the body feels and connecting it to an emotion is what motivates purposeful self-regulation behaviours. However, children and adults with autism, ADHD, sensory processing disorder, PTSD and more may have increased difficulties in being aware of their interoceptive senses. As a result, this would impact their ability to self-regulate effectively. Children in particular, may have more challenges with noticing their body signals and identifying their emotions. For example, a child has difficulties identifying their body signals such as clenched jaw, tight fist, and a headache prior to feeling angry and dysregulated. This will impact their ability to self-regulate and may lead to behaviours including throwing, yelling and kicking.
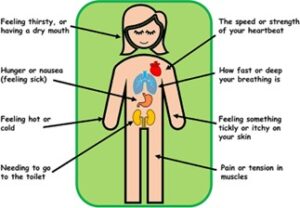
Figure 1: Homeostatic emotions in our body (Barker et.al, 2021)
How does interoception impact our daily life?
Difficulties with interoceptive awareness may lead to significant challenges in our day-to-day life and impact our engagement with our community. Listed below are some possible challenges a person with poor interoceptive awareness may experience:
- The person has difficulties identifying that they are getting overwhelmed until they are REALLY overwhelmed.
- Children and adults may have difficulties with regulating their other senses which can cause sensory dysregulation.
- The child can only recognise that they are feeling intense emotions such as anger and sadness when they are REALLY angry. This will cause difficulties with regulating their emotions appropriately.
- The person may forget to eat and drink for long periods of time because they cannot feel hungry or thirsty.
- The person can eat large amounts of food without feeling full or eats to the point where they feel sick or uncomfortable.
- They might not often feel the need to urinate or defecate until it is a last-minute emergency.
- They may not feel pain when they are injured and does not often notice when they are sick.
- Most often they have difficulties recognising when they feel tired and need to go to bed.
- Occasionally the person is very sensitive to changes in temperatures (Mahler,2019).
Developing Interoception skills at home:
So, what can we do to teach ourselves to read and understand our secret body signals. Below are some ideas that you can try with your children or by yourself:
- Yoga (focuses on how the mind and body feels)
- Mindfulness (focus on emotional regulation)
- Breathing exercises (calming and helps with attention
- Heavy work activities (to provide deep pressure movements in our joints to support with regulation)
- Alerting activities e.g., running, jumping, climbing and more.
- Practice identifying different sensations (e.g., hot cold, sweaty, dry, shaky, itchy, fast, slow, clenching)
In addition, before completing the running activity, ask your child to feel their heartbeat and pulse. Verbally prompt them to identify the feeling in their body. For example, “Is your heart beating slow or fast” or “are you breathing slowly or fast”. Once running activity is completed, ask them again to see if they noticed any changes in their body.
Reference: Mahler, K 2019, The interoception curriculum, United States of America
Tia Hafiza – Occupational Therapist
- Building blocks of literacy development
- What is phonological awareness?
- Phonological awareness skill hierarchy
- Tips for literacy and phonological awareness skill development at home
Building blocks of literacy development
From the first few months of life, children’s literacy experiences begin to build a foundation for later reading and writing success. From 2-4 years, children show rapid growth in literacy. They begin to “read” their favourite books by themselves, focusing mostly on the pictures. Eventually, at 3-4 years old they progress from talking about each picture individually to linking the pictures into a story, using language that sounds like “reading” or written language.
At this time, children also experiment with writing by forming scribbles, letter like forms, and random strings of letters. When using these forms of writing, children are trying to create meaning and will often “read” their printed messages using language that sounds like reading.
For children to begin reading and writing specific words they require the development of several skills, including:
- Phonological awareness
- Decoding – alphabet, sound, and symbol knowledge
- Ability to spell and recognise sight words
- Ability to infer and understand words, sentence structure and context
- Ability to speak (oral language)
- Print awareness and knowledge (e.g., what is a word, sentence, title, author, front and back of a book, etc.)
- Executive functioning (memory, planning, thinking, problem solving), and
- Execution (e.g., holding a pencil to be able to write letters)
Speech pathologists collaborate with children’s teachers and school support officers to determine goals for literacy, reading and spelling development, mainly working on one or more phonological awareness skills. Speech pathologists can work with school staff to provide specialist teaching in the area of language and phonological awareness.
What is phonological awareness?
Phonological awareness is the awareness of and ability to “tune-in” to the sound structure of spoken language, to become aware of sounds and their varying positions in words.
It includes:
- Awareness of rhyme
- Awareness that words can be broken down into syllables, sentences can be broken down into words and words can be broken down to separate sounds.
- Awareness of sounds in a language
- Ability to separate sounds in words
It is important for children to have phonological awareness to be able to develop literacy skills for reading and writing.
Phonological awareness skill hierarchy
Children develop their phonological awareness by developing their skills in the following:
- Syllable awareness and rhythm – the ability to identify the beats in a word e.g., the beats in helicopter are he-li-kop-ter
- Rhyme awareness and production – the ability to identify when words have the same sound ending and be able to produce a word with the same sound ending as another, e.g., cat rhymes with hat and mat
- Initial and final sound sorting – the ability to sort words into groups based off the sounds they start with or end with e.g., little goes with lake, pan with man
- Onset-rime segmentation – the ability to break words into two parts; the first sounds they start with and the rest of the word e.g., tap – t (onset) ap (rime), plum – pl (onset) um (rime)
- Initial and final sound identification – the ability to name the sound at the start or end of a word e.g., dog begins with the d sound and ends in the g sound.
- Blending sounds into words – the ability to brings sounds together to make words e.g., the sounds c, a, t make the word cat.
- Segmenting words into sounds – the ability to separate a word into its sounds e.g., the sounds in the word moon are m, oo, n.
- Deleting and manipulating sounds – the ability to take out, add or change the sounds in a word to make it into another word e.g., replace the sound b in book with the l sound to make look, or take out the r sound in broom to make boom.
Tips for literacy and phonological awareness skill development at home
- Read at minimum one book a day to your child, e.g., each night before bed. Start with simple picture books. Introduce books with text/story (around 2 usually).
- Provide them with many books among their toys to spark interest and look at the pictures
- Build your child’s print awareness – help them understand where the title, author, front and back of the book is, recognise some letters, that reading is left to right
- Once 2-4 years old, teach them what a letter, sound, word and sentence mean
- Share literacy-based activities with them e.g., shopping lists, recipes, chore lists, calendar reminders etc.
- Support reading with conversations about what the book was about during and after
- Sing nursery rhymes – exposes children to rhyme
- Read Dr Suess books – develops children’s rhyming abilities
- Play games during everyday routines e.g., while driving in the car, at the shops, mealtimes, and bath times etc.
- Play hangman
- Clap out the beats in words
- Take turns thinking of words that rhyme with another and see if you can make a long list with your child
- ISpy – help build awareness of the first sound in a word
- Pick a word and break it into its first sound and the rest of the word or have fun manipulating it by changing, taking out and/or adding sounds in the word to make new words – can use a white board, magnet letters on the fridge or printed letters to do this
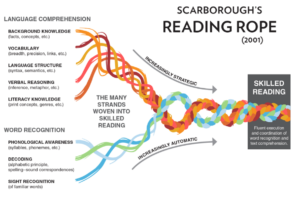
See below for a visual representation of the building blocks for literacy called ‘Scarborough’s Reading Rope’.
If you have any questions or concerns about you child’s literacy skills and phonological awareness, please speak to your local general practitioner.
Sarah Colangelo – Speech Pathologist
In mid Oct 2022, Bounce Back Health had the lovely privilege hosting Mandy Roscher from Physio Skills to teach other physios about women’s pelvic health. Mandy travelled from Brisbane to Adelaide to teach 13 other lovely physios who also travelled near and far to learn more about women pelvic health.
From the course we learnt about:
How to refine our subjective assessments
Urinary Incontinence (Stress, Urgency & Mixed)
Refined our internal vaginal assessment skills
How to complete an external rectal assessment
Prolapses
Trauma and pelvic health
Communication skills
Something key that was taken from the course is how vulnerable our pelvic floor is and how interconnected all our bodily systems are! What was also interesting to take note of was, even though you may not experience pelvic pain, internal assessments can cause some post discomfort which really put into perspective how some of clients feel.
It was such a lovely weekend filled with lots of learning and knowledge. We are so excited to put into practice what we’ve learnt so we can help as many people as we can! We have such a lovely little women’s health department! We would love to share our knowledge and help you if we can!
Fiona Pham – Women’s Health Physiotherapist


Exciting January School Holiday Groups at Bounce Back Health!
Dear Families,
Our fun and supportive January School Holiday Group programs are starting soon – perfect for building skills, making friends, and having a great time!
Here are the details:
Primary School Prep (Ages 4-5) Tuesdays: 6th, 13th & 20th January Time: 12:30pm - 2:30pm
High School Preparation Tuesdays: 6th, 13th & 20th January Time: 12:00pm - 2:00pm
These school prep sessions are ideal for kids entering primary or high school in 2026, or those who transitioned in 2025 and could use extra support!
Junior Chefs Thursdays: 8th, 15th & 22nd January Time: 10:00am - 12:00pm
Video Games (Ages 7-13) Monday 5th January: 11:30am - 1:00pm Wednesday 21st January: 10:00am - 11:30am
Lego Masters Mondays: 5th & 19th January Time: 2:00pm - 3:00pm
Spaces are limited – please let us know ASAP so we can arrange enough clinicians to support the groups!
NDIS funding may apply. Secure your child’s spot today! Call: (08) 8520 6244 Email: infoge@bouncebackhealth.com.au
FOR ADITTIONAL DETAILS / BOOKING: bouncebackhealth.com.au/class-types/school-holiday-programs/ ... See MoreSee Less
0 CommentsComment on Facebook
... See MoreSee Less
0 CommentsComment on Facebook
📘 What is a Learning Disorder?
A learning disorder is not the same as Autism or ADHD. It means a child
may have difficulties in specific areas like reading, writing, spelling,
or math — even though their overall intelligence is not affected.
❗ Why it matters:
Sometimes parents notice their child struggling at school and think
they’ll “grow out of it.” But if left unsupported, learning
disorders can affect confidence, school attendance, anxiety, and
long-term challenges in daily life.
🎯 The good news:
With the right strategies, children can learn in ways that work for
them. Occupational Therapists (OTs) are highly skilled in supporting
children with learning disorders by building the foundations for
attention, memory, motor skills, and classroom success.
Want personalized support? At Bounce Back Health, our experienced
Occupational Therapists love to help children and adults build life-changing
skills.
📞 Call us: 08 8520 6244
📧 Email: infoge@bouncebackhealth.com.au
#LearningDisorders #Dyslexia #Dysgraphia #Dyscalculia #ChildDevelopment
#OccupationalTherapy #BounceBackHealth #NDISProvider #SchoolSupport
#EarlyIntervention ... See MoreSee Less
0 CommentsComment on Facebook
✨ CREATE A CALM BOX ✨
A simple but powerful tool to support emotional
regulation at home in a quiet space. Fill a box with comforting items—like fidgets,
soft toys, calming scents, or favourite music. When big feelings arise, encourage
children (or adults!) can use their calm box to ground themselves, feel
safe, and regain control. 🌈💛
Want personalized support? At Bounce Back Health, our experienced
Occupational Therapists love to help children and adults build life-changing
skills.
📞 Call us: 08 8520 6244
📧 Email: infoge@bouncebackhealth.com.au
#emotionalregulation #calmbox #OccupationalTherapy #childdevelopment
#NDIS #ParentSupport #autismsupport #sensorystrategies #BounceBackHealth ... See MoreSee Less
0 CommentsComment on Facebook
Understanding big emotions can be tough, but what if we made learning about
them a fun game?
One of our favourite ways at BBH to do this is with "Pretend
Play with Emotion Faces."
How to do it at home:
* Gather some paper, markers, and craft sticks.
* On the paper, draw a bunch of faces
showing emotions—happy, sad, angry, surprised, silly, scared, etc
* Cut them out and tape on a stick
* Time to play! Now, you can use these faces in a few ways. You can
take turns making the sound that goes with each emotion, or tell a short
story using a few of the faces. Another fun idea is to have your child
pick a face and tell you about a time they felt that way.
This simple activity helps children recognize and express their feelings
in a safe and playful way. It teaches them that all emotions are okay
and gives them the language to talk about how they feel.
Need more support?
Want personalized support? At Bounce Back Health, our experienced
Occupational Therapists love to help children and adults build life-changing
skills.
📞 Call us: 08 8520 6244
📧 Email: infoge@bouncebackhealth.com.au
#EmotionalRegulation #OccupationalTherapy #ChildDevelopment
#KidsActivities #SocialEmotionalLearning #SensoryPlay #ParentingHacks
#BounceBackHealth #Gawler #SouthAustralia ... See MoreSee Less
0 CommentsComment on Facebook